Rewiring the Mental Healthcare System: Our Seed and Series A Investment in Headway

Seven years ago, I turned to in-person therapy to deal with a sudden crisis in my personal life. I emerged from that ordeal a strong believer and advocate for the efficacy and importance of therapy. Even in the short timespan since then, many more people are speaking out about their struggles with mental health. Without this public conversation, the problem had largely flown under the radar, but today employers, governments, and insurance companies are giving mental health the attention it deserves for the first time. What hasn’t changed, unfortunately, is the affordability and access crisis that continues to plague this critical aspect of our healthcare.
Therapy is expensive. Each of my visits cost $150 out-of-pocket each week, which means that my monthly bill was more than the average American has saved for an emergency expense. It is a national embarrassment that accessing mental health care is so prohibitively expensive. I was privileged to be able to afford the care I needed, but I had to dip into my savings to do so. Therapists are largely individual practitioners and rarely opt into accepting health insurance, choosing instead to remain out-of-network to avoid the administrative burden of insurance. As a result, even health plans that cover mental health services don’t do much to address mounting costs.

We are in the middle of a mental health crisis in this country. Millions are suffering from isolation, depression, trauma, anxiety, or even more serious disorders — all of which have been exacerbated by the global pandemic and social unrest we are experiencing. I have lived in the heart of San Francisco for the past decade, where this crisis is on full display. It’s painfully obvious that, left unaddressed, there will continue to be severe downstream consequences for individuals, for families, and for society writ large.
I first started looking into mental health as an investable category two years ago, when a talented and mission-driven engineer I know eschewed a compelling offer from a top-tier tech company to work on a mental health app. My work on the space eventually led me to Andrew Adams and Headway in December 2018. I was struck by how problem-obsessed he was and how aligned our views were on affordability and access. He had challenged the core assumption in the space — that therapists wouldn’t accept insurance — by providing software to automate the process and alleviate this friction. Even though Headway was piloting their product with only a handful of therapists, the early results proved to me that the model could work.
In the summer of 2019, Accel led Headway’s seed round and I joined the company's board of directors. In the year since our investment, that nascent product-market fit has turned to aggressive growth. There are currently over 1500 therapists on Headway’s platform and an even faster growing number of patients served. By bringing therapists in-network while not compromising quality of care, we have found a way to make therapy significantly cheaper — in some cases 10x cheaper — which dramatically impacts who can access it. I know we’re doing something right when the most common employer among our patients is the New York MTA, not a company paying tech salaries. Demand for mental health care has always been there, but now with Headway, more people can finally get the care they need.
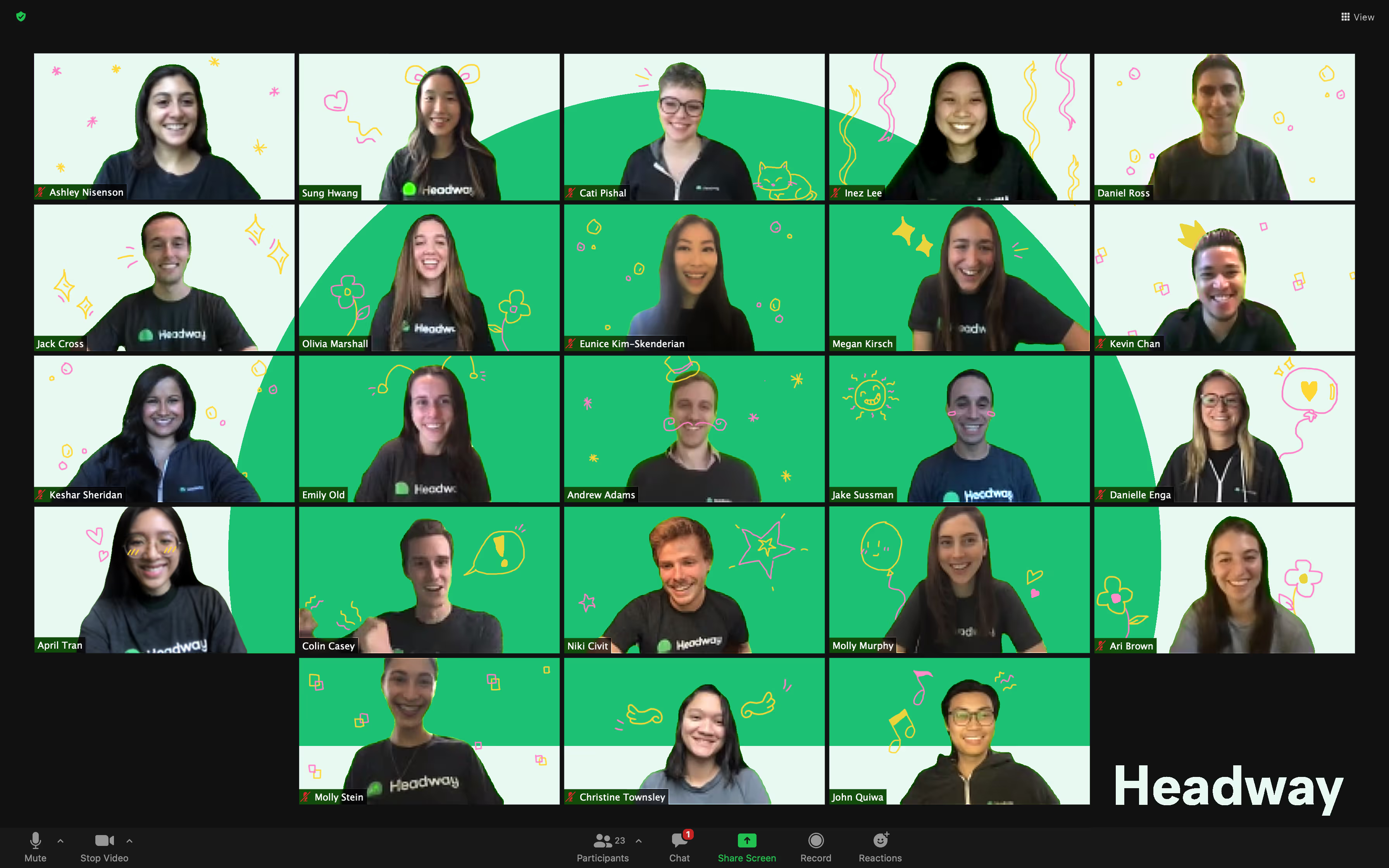
Today, we are thrilled to welcome seasoned healthcare investors Thrive Capital and GV to Headway as we announce a $26m Series A financing. Accel, of course, is doubling down on its original investment and participating. I am encouraged by the validation this financing brings, the incredible mission-driven talent that has joined us on this journey, and the momentum we’re seeing as payers, providers, and patients embrace what we’re building. But perhaps more importantly, I am genuinely proud to work on such a meaningful problem alongside Andrew and his-cofounders Jake Sussman, Dan Ross, and Kevin Chan, as the story of mental healthcare is rewritten over the next decade.
Great companies aren't built alone.
Subscribe for tools, learnings, and updates from the Accel community.


